Original post written on 4th June 2023 by Giuseppe Natalini
Mario and Pippo have an infection which also causes hypotension. After an initial fluid administration, they present as follows:
-Mario, 45 years old, no chronic disease. Blood pressure: 78/48 mmHg (mean arterial pressure 58 mmHg).
-Pippo, 75 years old, receiving treatment for arterial hypertension. Blood pressure: 95/50 mmHg (mean arterial pressure 67 mmHg).
Based on this limited information, let's try to ask a couple of questions:
1) Are these data sufficient to decide whether to intervene to increase Mario and/or Pippo's blood pressure, and if so, by how much?
2) Do you think there are other data to consider in order to answer the question?
Before attempting to answer these questions, let's consider both data from clinical studies on arterial pressure in septic shock and the
physiological basis of arterial pressure.
What do clinical studies say?
The latest edition of the Surviving Sepsis Campaign guidelines recommends that, in adults with septic shock, mean arterial pressure should initially be targeted to reach 65 mmHg (compared to higher targets) (1).
However, when considering clinical studies in patients with septic shock as a whole, they do not support the idea that there is a threshold value of mean arterial pressure to be reached.
It should be noted that the clinical and physiological impact of mean arterial pressure values below 60-65 mmHg has not been studied. Therefore, the value of 65 mmHg should be considered as the lowest of the values which were studied.
When 65 mmHg of mean arterial pressure is compared to higher values (mostly between 75 and 85 mmHg), the studies reach conflicting conclusions: in some cases, there are no differences in outcomes, in others, it may be more favorable to maintain lower values, and in others, higher levels of pressure seem to be more favorable (2-8).
Considering these conflicting results as a whole, one should consider the idea that mean arterial pressure is probably a not so important target for cardiovascular support of patients with sepsis.
Arterial pressure, physiological aspects.
Arterial pressure during the cardiac cycle.
A premise: in our reasoning, we will completely ignore the retrograde reflection of the pressure wave, which is a very important aspect in the formation of the arterial pressure wave. However, omitting it does not alter the meaning of the reasoning we will present.
Arterial pressure is the result of the stretching of the elastic fibers of the arterial wall caused by the volume of blood contained within.
The volume of blood contained in an artery at any given instant is determined by the dynamic equilibrium between two flows: one coming from the heart and one going towards the peripheral circulation.
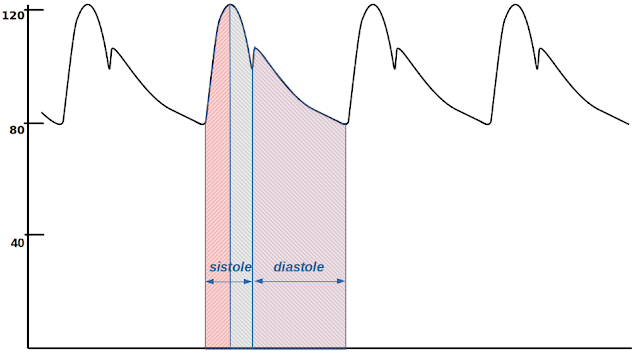
During systole, these two flows are present simultaneously, meaning that blood arrives from the heart and blood exits towards the peripheral circulation at the same time. In the initial phase of systole (red area in Fig. 1), pressure increases because the volume of blood in the artery increases, meaning that incoming flow is greater than outgoing flow.
Figure 1
This increase in volume is accommodated by the systolic expansion of the artery, which reaches its maximum at the systolic peak (Figure 2).
Figure 2
As systole progresses beyond the systolic peak, the pressure decreases, indicating that the volume of blood in the artery decreases. The inflow continues, but now the outflow exceeds it (gray area in Figure 1).
The dicrotic notch marks the transition from systole to diastole (lilac area in Figure 1): the closing of the aortic valve stops the inflow to the artery, and only the outflow remains. Therefore, diastolic arterial pressure expresses the interaction between the arterial vessel and the peripheral circulation, unlike systolic arterial pressure, which also includes coupling with the cardiac pump.
The diastolic flow from the artery to the peripheral circulation is propelled by the elastic recoil of the arterial wall against the volume of blood contained within it (Figure 3) and hindered by downstream pressure.
Figure 3
Let's now try to understand the meaning of this downstream pressure, which is also crucial for the correct interpretation of mean arterial pressure.
Usually, diastole lasts less than 1 second and is interrupted by the next systole. Let's imagine that we could extend diastole for several seconds, allowing the complete outflow of arterial blood towards the capillary circulation and achieving a complete cessation of arterial flow. How low do we think arterial pressure could drop during this hypothetical extended diastole? It has been theoretically and experimentally demonstrated that the reduction in diastolic arterial pressure stops at pressure values which are significantly higher than those of venous pressures, typically around 25-50 mmHg (9-11). This is considered a critical closing pressure, below which the flow ceases, and consequently, tissue perfusion is halted.
At this point, it becomes clear that the entire portion of diastolic arterial pressure below the critical closing pressure should not be considered as perfusion pressure.
Furthermore, diastolic arterial pressure is dependent on peripheral vascular resistances, primarily located at the pre-capillary arteriolar level. As a result, diastolic arterial pressure can decrease slowly (and therefore remain elevated) due to arteriolar vasoconstriction, which hinders blood outflow (and tissue perfusion). Alternatively, it can decrease rapidly (and therefore become immediately low) if there is vasodilation, facilitating perfusion and blood flow towards tissues.
It is therefore evident that only a portion of the diastolic arterial pressure (that above the critical closing pressure) generates flow, and this portion of diastolic arterial pressure can even have an inverse relationship with flow itself.
Unlike diastolic pressure, pulse pressure (the systolic pressure increment) is directly correlated to stroke volume and, therefore, to cardiac output and perfusion. The extent of the correlation between pulse pressure and stroke volume depends, obviously, on arterial compliance. For example, the same stroke volume may generate a pulse pressure that increases in parallel with age.
Mean arterial pressure
In Figure 4, a "normal" arterial pressure curve is depicted, with a systolic pressure (SBP) of 122 mmHg, and a diastolic pressure (DBP) of 80 mmHg. The pulse pressure (PP) is 42 mmHg.
Figure 4
Mean arterial pressure is the average pressure during a complete cardiac cycle (systole and diastole). It is calculated by dividing the area under the pressure curve during one cardiac cycle by the duration of the cycle (red area, equivalent to the gray area in Figure 4). When blood pressure measurements are taken frequently (e.g., during invasive blood pressure monitoring with at least 100 samples per second), mean arterial pressure can be approximated well by the arithmetic mean of all the measured pressure values throughout the cardiac cycle.
Mean arterial pressure (MAP) can also be estimated (approximately) using the equation:
MAP=SBP+1/3⋅PP (eq. 1)
In the example shown in Figure 1, the calculated MAP is 94 mmHg.
As can be seen both from the graphical evaluation in Figure 4 and from Equation 1, mean arterial pressure is primarily determined by diastolic arterial pressure and to a lesser extent by pulse pressure. In our example, out of the 94 mmHg of mean pressure, 85% is due to diastolic pressure (80 mmHg) and only 15% to pulse pressure (the remaining 14 mmHg).
Mean arterial pressure combines diastolic and pulse pressure, which, however, have very different physiological and hemodynamic meanings. Within MAP, the diastolic component, which is the part of arterial pressure that is less correlated with tissue perfusion, carries more weight.
Given these considerations, it is not surprising that clinical studies have not led to a clear target for mean arterial pressure in the treatment of patients with shock.
Let's get back to Mario and Pippo...
Now we can address the first of our two initial questions, which asks whether and how we should modify the blood pressure for Mario (a healthy forty-five-year-old with a mean arterial pressure of 58 mmHg) and/or Pippo (an hypertensive seventy-five-year-old with a mean arterial pressure of 67 mmHg). The answer is disappointingly simple: we don't have enough data to make a decision. Blood pressure is an easily measurable parameter but of limited clinical utility in a patient with shock. The blood pressure of both Mario and Pippo could be sufficient for organ and tissue perfusion, or it could be inadequate.
We necessarily need additional information to decide whether and what actions should be taken. This would be the second question to answer, but this post has already become quite lengthy. It's worth taking a break and continuing in the next post.
Conclusions
Let's summarize the main concepts discussed in today's post:
-Achieving a mean arterial pressure of 65 mmHg is considered a treatment target for patients with hypotension secondary to infection, but the literature presents conflicting conclusions on this matter.
-Pulse pressure is also influenced by stroke volume, which forms the basis of cardiac output and is therefore an important factor in peripheral perfusion.
-Diastolic blood pressure is dependent on peripheral vascular resistance and the critical closing pressure, which limit the flow towards tissues.
-In calculating mean arterial pressure, the weight of diastolic pressure is predominant compared to pulse pressure. Since perfusion (cardiac output) is influenced by pulse pressure and not diastolic pressure, it is reasonable to consider mean arterial pressure as an unreliable indicator of perfusion. This understanding sheds light on the inconclusive results of clinical studies in search of the "right" mean arterial pressure.
-To assess hemodynamic adequacy in patients with shock, it is essential to consider additional perfusion indices alongside blood pressure measurements.
As always, warm regards and a smile to all of ventilab‘s friends.
References:
1) Evans L, Rhodes A, Alhazzani W, et al.: Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med 2021; 47:1181–1247
2) LeDoux D, Astiz ME, Carpati CM, et al.: Effects of perfusion pressure on tissue perfusion in septic shock: Crit Care Med 2000; 28:2729–2732
3) Bourgoin A, Leone M, Delmas A, et al.: Increasing mean arterial pressure in patients with septic shock: Effects on oxygen variables and renal function: Crit Care Med 2005; 33:780–786
4) Thooft A, Favory R, Salgado D, et al.: Effects of changes in arterial pressure on organ perfusion during septic shock. Crit Care 2011; 15:R222
5) Asfar P, Meziani F, Hamel J-F, et al.: High versus Low Blood-Pressure Target in Patients with Septic Shock. N Eng J Med 2014; 370:1583–1593
6) Lamontagne F, Meade MO, Hébert PC, et al.: Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Medicine 2016; 42:542–550
7) Lamontagne F, Richards-Belle A, Thomas K, et al.: Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA 2020; 323:938
8) Maheshwari K, Nathanson BH, Munson SH, et al.: The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med 2018; 44:857–867
9) Permutt S, Riley RL: Hemodynamics of collapsible vessels with tone: the vascular waterfall. J Appl Physiol 1963; 18:924–932
10) Kottenberg-Assenmacher E, Aleksic I, Eckholt M, et al.: Critical closing pressure as the arterial downstream pressure with the heart beating and during circulatory arrest: Anesthesiology 2009; 110:370–379
11) Maas JJ, de Wilde RB, Aarts LP, et al.: Determination of vascular waterfall phenomenon by bedside measurement of mean systemic filling pressure and critical closing pressure in the intensive care unit: Anesth Analg 2012; 114:803–810